Depression is a debilitating mental health condition affecting millions of individuals worldwide. While traditional antidepressant medications and therapy can be effective, some individuals may not experience relief from their symptoms or may have to wait several weeks for the effects to take hold. In recent years, ketamine therapy has gained attention as a novel treatment due to its potential to rapidly alleviate symptoms of depression.
In this article, we will explore what ketamine therapy is, its uses, how it compares to other experimental treatments, its cost, administration methods, the experience of ketamine therapy, and the ideal candidates for this treatment.
What is ketamine therapy for depression?
Ketamine therapy involves the administration of a low dose of ketamine, an anesthetic medication, to treat symptoms of depression. While ketamine has long been used for anesthesia and pain management, recent research published by the National Institutes of Health (NIH) reveals it may have the potential to rapidly reduce depressive symptoms in certain individuals, particularly those who have not responded to traditional treatments.
The primary uses of ketamine therapy include:
- Treatment-Resistant Depression: Ketamine therapy shows promise for providing relief in individuals with treatment-resistant depression where other medications and therapies prove ineffective.
- Acute Suicidal Ideation: Ketamine can rapidly reduce suicidal thoughts and provide short-term relief in individuals experiencing acute suicidal ideation.
- Bipolar Depression: Studies have suggested that ketamine may also be effective in treating depressive symptoms associated with bipolar disorder.

How ketamine therapy works
Ketamine therapy involves the administration of a low dose of ketamine, an anesthetic medication, to alleviate symptoms of depression. The exact mechanisms by which ketamine exerts its antidepressant effects are not fully understood, and ketamine therapy is still an area of ongoing research.
However, current research suggests several possible mechanisms:
- Glutamate Modulation: Ketamine primarily acts on the glutamate system, which is the most abundant neurotransmitter in the brain. It blocks certain receptors, increasing the release of glutamate in the synaptic space. This increase in glutamate availability and transmission is believed to enhance synaptic connections and promote neuroplasticity, which can positively influence mood regulation.
- Synaptic Remodeling: Ketamine’s effects on glutamate transmission can trigger a cascade of events that promote the growth and strengthening of synapses (the connections between brain cells). This process, known as synaptic remodeling or synaptogenesis, facilitates new neural connections, which helps restore proper brain circuitry and alleviate depressive symptoms.
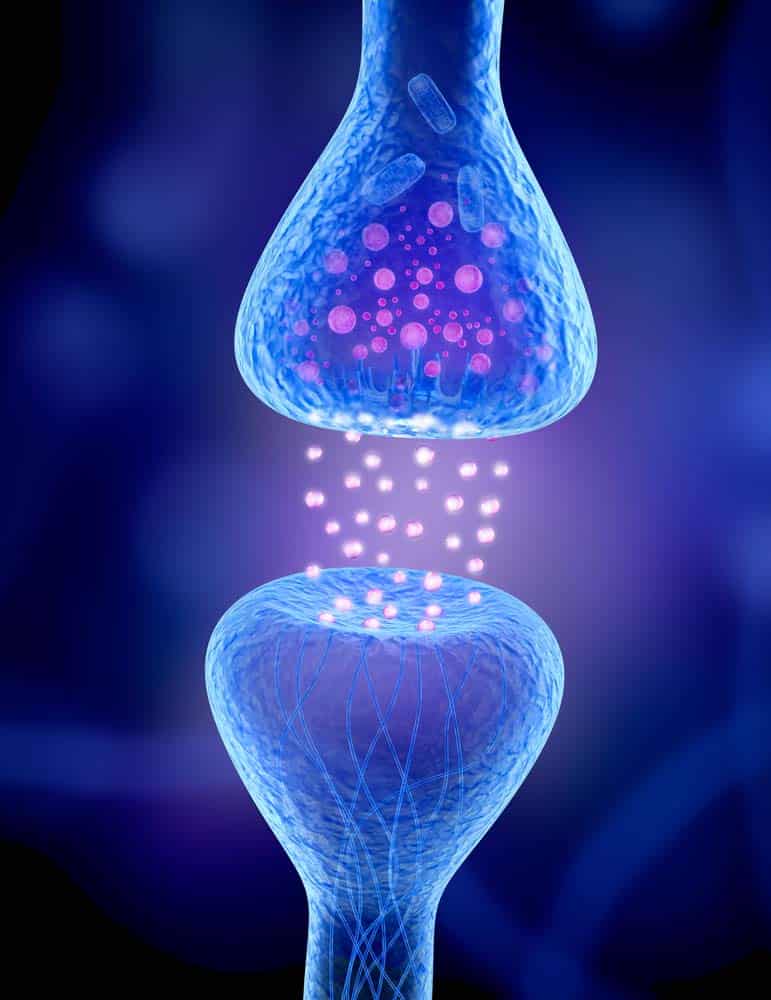
- Neurotrophic Factors: Ketamine administration causes increased levels of brain-derived neurotrophic factor (BDNF), a protein that supports the growth and survival of neurons. BDNF is essential for neuroplasticity, and its upregulation may contribute to the antidepressant effects of ketamine.
- Anti-inflammatory Effects: Some studies suggest that ketamine therapy may have anti-inflammatory properties. Chronic inflammation in the brain is a known cause of depression, and by reducing inflammation, ketamine may help improve symptoms. However, further research is needed to fully understand the extent of ketamine’s anti-inflammatory effects.
It’s important to note that the effects of ketamine therapy are relatively rapid compared to traditional antidepressant medications. While traditional antidepressants often take weeks to produce noticeable effects, ketamine therapy can lead to a reduction in depressive symptoms within hours or a few days after treatment.
HOW IS KETAMINE THERAPY ADMINISTERED?
Ketamine therapy can be administered through different methods, with the most common being intravenous (IV) infusion. The administration method may vary depending on the healthcare provider’s preference and an individual’s specific needs.
The main methods of ketamine administration in therapy include:
- Intravenous (IV) Infusion: This is the most common and widely used method of ketamine administration in therapy. A small needle is inserted into a vein, typically in the arm, and a controlled dose of ketamine is delivered through an IV drip. This allows for precise control over the dosage and the rate at which the medication enters the bloodstream. IV infusion also allows healthcare providers to monitor the patient closely during the session.
- Intramuscular (IM) Injection: In some cases, ketamine may be administered via an intramuscular injection. This method involves injecting the medication into a large muscle, such as the thigh or buttock. Intramuscular injection may be used when IV administration is not feasible or preferred. However, it’s important to note that this method may have a different absorption rate and may require careful monitoring.
The healthcare provider will determine the exact dosage and infusion rate of ketamine based on several factors, including the individual’s weight, medical history, and specific treatment goals. The aim is to provide an effective dose that produces therapeutic effects while minimizing potential side effects.
During ketamine therapy sessions, healthcare professionals monitor vital signs, such as blood pressure, heart rate, and oxygen levels, to ensure the safety and well-being of the patient. The duration of a ketamine therapy session can vary, but it typically lasts around 40 minutes to an hour.
Who is a good candidate for ketamine therapy?
Ketamine therapy can be beneficial for a range of individuals experiencing depression. However, it is important to consider certain factors when determining the ideal candidates for this therapy.
While each case needs to be evaluated on an individual basis by a qualified healthcare professional, there are some general considerations:
- Treatment-resistant depression: Ketamine therapy is often considered for individuals who have not found relief from traditional antidepressant medications or other therapies. It can provide an alternative option for those who have not experienced significant improvement in their depressive symptoms despite trying multiple treatment approaches.
- Acute suicidal ideation: Ketamine has shown rapid and promising effects in reducing acute suicidal ideation. Individuals experiencing intense suicidal thoughts or immediate risk may be considered good candidates for ketamine therapy due to its potential for providing short-term relief and stabilizing their mental state.
- Bipolar depression: Some research suggests that ketamine may be effective in treating depressive symptoms associated with bipolar disorder. Individuals with bipolar depression who have not responded adequately to other treatments may be considered for ketamine therapy.
- Urgency for symptom relief: Ketamine therapy is particularly suitable for individuals who require a rapid reduction in depressive symptoms. It can offer a more immediate response compared to traditional antidepressant medications, which often take several weeks to reach their full effect.
Ketamine therapy MAY NOT be suitable for those with the following factors:
- Uncontrolled high blood pressure or certain heart conditions
- Pregnancy or breastfeeding
- History of substance abuse or psychosis: Ketamine has the potential for misuse and may not be recommended for individuals with a history of substance abuse or psychosis. Close evaluation and consideration of individual circumstances is necessary in these cases.
It is important to consult with a qualified healthcare professional or mental health provider to evaluate your individual situation and determine if ketamine therapy is a suitable treatment option for you. They will assess your medical history, current medications, and overall health to make an informed decision and develop a personalized treatment plan.
How ketamine therapy compares to other experimental treatments
Ketamine therapy and psilocybin therapy are both emerging treatment approaches for mental health conditions, but they have distinct differences in terms of mechanism of action, treatment protocols, and research stages.
Whereas ketamine primarily modulates the glutamate system in the brain, leading to enhanced synaptic connections and neuroplasticity, psilocybin, the active compound in “magic mushrooms,” interacts with the serotonin system in the brain. Psilocybin binds to serotonin receptors and influences various neural networks, leading to altered perception, cognitive effects, and potentially therapeutic benefits.
Ketamine has been studied extensively and progressed further in terms of research and clinical applications. In 2019, the U.S. Food and Drug Administration (FDA) approved esketamine (an isomer of ketamine) for specific indications like treatment-resistant depression. Psilocybin therapy is still in the early stages of research and clinical trials. Although promising results have been reported, it has not yet received regulatory approval for therapeutic use.
What else might ketamine therapy treat?
In addition to depression, ketamine therapy shows potential for treating several other conditions.
While further research is needed to establish its effectiveness and safety for these indications, some areas of interest include:
- Anxiety disorders, including generalized anxiety disorder (GAD), post-traumatic stress disorder (PTSD), and social anxiety disorder (SAD).
- Postpartum depression
- Substance use disorders
- Chronic pain conditions, such as fibromyalgia, neuropathic pain, and complex regional pain syndrome (CRPS).
It’s important to note that while ketamine therapy may show promise for these conditions, more research is needed to establish its safety, efficacy, and optimal treatment protocols. The use of ketamine for these indications may be considered off-label, and individualized assessment and careful monitoring by qualified healthcare professionals are essential.
How much does ketamine therapy typically cost?
The cost of ketamine therapy varies depending on several factors, including the location, clinic, and treatment duration. On average, a single ketamine therapy session can range from $400 to $800. However, multiple sessions are typically required to achieve the best results. The number of sessions needed will vary depending on the person’s response to treatment and the severity of their depression.
In addition to the session cost, there may be fees associated with the initial consultation, medical assessments, and any necessary follow-up appointments. Additionally, the cost of ketamine therapy may not be covered by all insurance plans, as it is still considered an experimental treatment for depression.
Enterhealth's Stance on Ketamine Therapy
At Enterhealth, we’ve treated people for substance use disorders and addiction for more than 15 years, and that includes ketamine use disorders. However, we recognize that for certain individuals and under the administration of a certified medical practitioner, ketamine therapy may have the potential to help people suffering from treatment-resistant depression.
While we do not offer ketamine treatment as a part of our program, we do occasionally refer patients to outside practitioners who do offer it.
If you have any questions about our holistic addiction and mental health treatment programs, you can call us anytime at 800.388.4601 or visit our contact page to leave us a message.
Disclaimer: The information provided in this article is for informational purposes only and should not be considered as medical advice. Consult with a qualified healthcare professional before making any decisions regarding your mental health treatment.